What is chronic inflammation and how does celiac disease cause it to occur?
Celiac disease has been linked with several other diseases and conditions, most of which are related in some way to the inflammation caused by the disease. It’s simple enough to say celiac disease causes inflammation. Celiac patients often experience chronic inflammation symptoms that can accompany celiac disease. But just what is inflammation and how does celiac disease cause it to occur?
Ironically, inflammation is actually part of the body’s natural healing process. In a healthy person, inflammation is a sign that the body has sent its first line of defense – disease-fighting cells – to the site to help battle harmful pathogens and ward off infection. But in a person with an autoimmune disease like celiac disease, those cells turn against healthy cells, damaging tissues and organs and impairing the body’s normal functions.
Celiac disease is an autoimmune disorder, meaning that the body attacks itself. Hair-like structures (or finger-like structures) called villi line the small intestine, allowing nutrients to be absorbed into the bloodstream. When gluten is eaten, villi become inflamed and flattened. In people with damaged villi, vitamins, minerals, carbohydrate, protein and fat are poorly absorbed, causing nutritional deficiencies and health of the body is affected.
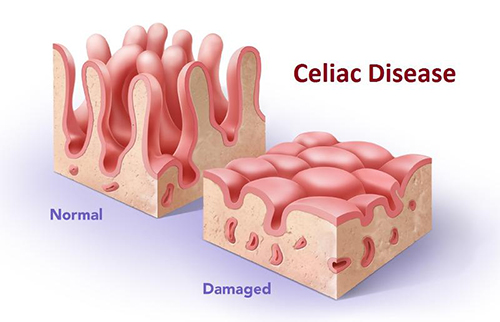
A detailed view of the villi, hair-like structures in the small intestine. At left, normal villi and at right, inflamed villi, damaged from celiac disease.
White blood cells, or leukocytes, are the disease-fighting cells with which most people are familiar. There are several types of white blood cells, including B cells, specialized cells whose sole task is to travel through the bloodstream looking for invaders. When they find a foreign body like a virus or bacterium, they attach themselves to the outside of the object and begin producing antibodies designed to destroy the invaders. Another type of white blood cell, called “killer cells”, seeks out invaders and kills them immediately. In healthy people, these and the other types of white blood cells can differentiate between “normal” cells in your body and harmful invaders, and they play critical roles in warding off disease; but in people with CD, these cells can misidentify harmless substances like food particles for dangerous pathogens, attacking the healthy lining of the small intestine instead.
No one is sure what causes this “mistaken identity” to occur, but it’s a feature not only of celiac disease, but of all autoimmune diseases. And bowel inflammation isn’t the only kind of inflammation that can occur as a result of celiac disease. Several studies have shown a link between CD and joint inflammation, and some research has shown that people with CD are at a much higher risk for developing joint pain. Interestingly, research studies have also shown that people who don’t have CD may still have joint inflammation related to gluten consumption, implying that gluten can cause different types of inflammation to occur.
Inflammation in CD causes other problems. Because it affects the small intestine which plays a prominent role in digestion, CD can cause nutritional deficiencies to develop, notably deficiencies in vitamins A, D, E and K and iron, calcium and folic acid. In turn, these deficiencies can result in a decline in overall health and an exacerbation of CD symptoms including joint and bowel inflammation.
Dietary supplements can help make up for these nutritional gaps, but one of the problems with supplements is that many so-called gluten-free products are processed in facilities that manufacture or process products containing gluten, resulting in cross-contamination from microscopic gluten particles. Even these minuscule amounts are enough to trigger an immune response in people with CD or gluten sensitivity. That means that the products you’re taking to help you stay healthy could actually wind up making your condition worse.
CeliVites by Gluten Free Therapeutics is targeted to replace the nutrients lost due to poor absorption. They are completely gluten free to offer people with CD the nutrients they need in the most absorbable form for both good health and peace of mind. In fact, GFT was founded by the mother of an adult child with celiac disease, so every product is developed from real firsthand experience and “know-how.” To see the complete lineup of CeliVites, visit the Gluten Free Therapeutics website.
This information is provided by GFT to inform and educate. It is not to be used as a substitute for medical advice. We recommend that this and any other medical questions be discussed with a medical health professional.
This original article is made possible by Gluten Free Therapeutics. Our mission is to educate, inform, and provide the most effective nutritional products possible to allow those with celiac disease and serious gluten intolerances to heal their bodies. CeliVites complete line of superior gluten free supplements includes multivitamin/multimineral supplements, iron supplements, and calcium supplements for people living with celiac disease. All CeliVites products are designed to help you heal, restore and rebuild your body, because going gluten free isn’t enough!
Comments ()













I wonder, initially my gastro dr, blamed my intestine issues on antibiotics, however I never had any issues before major steroid treatment for a severe allergic reaction. Like my Fibromyaglia, my conclusions are that steroids are the cause of so much health problems
Cheryl, if u have had steroid treatments over a long period of time you could possibly have Cushings Snydrome, depending on the length of time you remained in steroid treatment. My daughter was recently diagnosed with it after repeated steroid use for her asthma. I sincerely hope that is not your case. it is a debilitating illness with lots of visual body responses. good luck to you and I hope you feel better soon.
Cheryl, did you know that 3% of those who have Fibromyalgia may have Celiac Disease as well? I am one of them. When I had my blood test done, I was extremely high. If I did not eat a gf diet, I would run the risk of developing full blown Celiac Sprue. Don’t want that as husband’s was not detected before age 40. He developed cancer in the small intestine and needed a major operation called a whipple. That was two years ago. Our youngest daughter has as well & detected at age 12. Every other family member has been tested. I also have Hashimoto’s Disease which runs hand in hand with a lot of FM folks.
Julie, Thank you very much for your comment. It is important to know what our readers are experiencing and helps us develop article topics. We research our articles carefully and only provide fact based information that has undergone medical review. In light our your comment we may need to write an article about fibromyalgia and celiac disease. I am sure many readers will find your comment helpful. Thank you for sharing.
Is there a difference between Celiac Disease and Celiac Sprue? It appears that if diagnosed later in life, the harder it is to control the symptoms, even with a GF diet. I have so many different, strange medical problems or symptoms that are blamed on the Celiac Disease.
The hospital pharmacy where I go game me the generic of Simvastatin and Lipitor at the same time. I did not look them up because I take about 10 different meds a day and I just thought the extra medication was one the doctor had just prescribed for me. I took them both for 3 weeks and I became so sick I really thought I was going to die. From that time until now – 4 years later – I developed Celiac Sprue Disease and numerous other diseases. I know that this is what caused my health problems, but no doctor will state that having all of the cholesterol removed from my body caused my problems. I think that steroids are the cause for most of our health problems. I’m on disability and can hardly function and have developed fibromyalgia on top of everything else. I totally agree with you Cheryl – totally.
My almost 15-year old son was diagnosed with Celiac about 2-1/2 years ago. I’ve learned a lot about Celiac from this article, in particular the potential issues with joint pain. Thank you!!
Thank you Jen,
It is our company’s mission to educate and inform our readers. We provide medically based, meticulously researched articles. We know how hard it is to get accurate about celiac disease and we are gratified to see you found this article useful.
Thank you for your kind words.
To add to the comments, both my daughter and I have fibromyalgia and celiac disease. Even controlling the celiac doesn’t fix everything else. Of course, I was diagnosed in my late 50’s and she in her early 40’s, so some damage can’t be undone it seems. Thankful for GF foods and better labeling!
Thank you for your informative articles. I was diagnosed Celiac over 7 years ago and since then I have gone gluten free, dairy free, corn free, soy free and refined sugar free. I do a lot of work with food therapy for my wellness clients and my autistic son and have found that it really does make a difference what food you eat as well as the supplements my son and I take. I totally trust my Naturopath and what she has found to help me with what my body was lacking. Adding a probiotic and enzymes to my regime has helped tremendously. To also help with my constant body inflammation I have recently gone more vegetarian and have noticed a difference in the inflammation. Thanks again for keeping us informed.
Paulette,
Thank you for your comment. We love hearing from readers who appreciate the articles we write. As part of our mission to educate and inform we write original articles each week to educate the celiac population at no cost to them. There is quite a bit of ungrounded and unscientific information out there and we hope to help educate by providing information that is reviewed and approved by medical professionals who work with celiac and related autoimmune diseases. We encourage our readers to send us the topics that most concern them so we can address those issues if possible. It is readers like you and others who have thanked us who motivate us to continue in our mission.
Thank you for your kind and insightful comment.
Understanding Hashimoto’s & Celiacs go hand in hand. Could you add information with regard to th-1 & th-2 (cell & humoral immunity)?
I have Celiac and have a weight problem . My stomach is huge and I dont eat 3 meals and try to stay away from strach like potatoes.
Before I was dianoised with celiac I was thinner still over weight but now i am 210 5’3 any suggestions on how to loose the stomach. No surgery please.
PLEASE GIVE ME ADVICE I AH CELIAC HAVE GAINED WT AND AM BLOATED CANT LOSE WT NOW THANK YOU
The weight watcher program has helped me tremendously to lose my big stomach. I was on Lyrica for almost 7 years and took myself off of it. I felt it was no longer helping me. Joined weight watchers in May and have lost 35 pounds since where I could never lose anything at all before. I fact I would gain…
Very nice post. I certainly appreciate this website. daegfkcgkece
I believe there is definitely a strong link between thyroid diseases and CD. 3 years ago I had a tumor on my thyroid gland that had grown and compromised it entirely. I had A total thyroidectomy done and suddenly started experiencing a multitude of symptoms. My parathyroids went into shock, and a full year went by where my body was not responding or absorbing the thyroid replacement hormone. Therefore, for a year, my body was trying to function without the benefits that a thyroid normally gives your body. My bowel movements slowed, digestion slowed allowing for a buildup of bad bacteria, everything gradually started getting worse with my GI tract. After another 1+ year and numerous ER visits, and experimental drugs for Lyme disease, SIBO ( small bacteria intestinal overgrowth), lactose intolerance, fructose intolerance, IBS, and after 8 doctors and a biopsy I was finally diagnosed with celiac. The intestinal wall is slightly damaged therefore I am not absorbing my thyroid replacement medicine, thus the vicious cycle continues. I wish more research was able to be done on how to fix this issue. Just wanted to share in the hopes someone else can relate.
Hi there
I was diagnosed as celiac after a GS and CS however as I have a sever iron deficiency and I am losing an alarming amount of weight. Blood tests and stool tests were run at this time I myself requested celiac tests which all came back negative. However my celiac diet which I have been on since being diagnosed originally definitely help me my specialist then confirmed I have a bleeding gut and until further tests are run in February to continue on my celiac diet however to eat more which I seriously cannot achieve.i do bloat and do have chronic pain is there something I can take for this or should I leave my body to do its own thing for now.
many thanks Diana
Coming from a CD family, and being the first to recognize the problem (in my daughter at age 3, in myself age 50 – yes denial was strong), I am now in pain from the inflammation in my gut. Seems constant and without end. I have been GF for 15 years and am looking to find a way to calm the inflammation. Paleo seems the best choice, with some modifications for my GF, DF, seafood free diet. It’s pretty hard to find foods that I can eat that will help give me the proper nutrients – like omega 3’s. I’m looking into celi-vites to see if I can take them.
Karen P, I read that Emu oil contains the omegas 3,6,9 and 12s.
I discovered after 15 years of complaints of tummy upsets which got worse over time that at 55 I was Coeliac.
I can tie it to massive long term doses of NSAIDs.
Now I have carpal tunnel, tarsal tunnel and osteo in feet and I suspect Fibromyalgia.
A gluten free diet is the least of my problems as I can reproduce most things just as delicious.
I have learned heaps from these articles. Is there any chance you will be writing articles about best foods/worst foods. I understand there are ways to include the solanum foods…potato tomato etc so as to reduce their chances of producing inflammatory responses.