One Year After Your CD Diagnosis
The healing process can lead to questions
You received your diagnosis of celiac disease a year ago and have eagerly started a gluten-free diet. There’s a very steep learning curve at first but, as you get the hang of reading every ingredient label, you may wonder about how long it will be until you get better. What should you expect at your one year follow up visit? How will your physician monitor your progress? What is the best way to know if you are healing and how long will it take to repair the damage? We turned to the latest scientific research to answer these and other questions:
1. When will I feel better?
There’s good news and bad news! The good news is that the vast majority of celiac disease patients will start feeling better within a few weeks after starting a gluten-free diet. Symptoms will begin to lessen. Regeneration of your digestive tract may take a little longer but, as long as you remain committed to your gluten-free diet, you’re in with a good chance to make a full recovery. The keys to healing are total elimination of gluten and good nutritional support.
The bad news is this can be a long process which may take years. In fact, after 12 months, about half the patients still have at least one abnormality in their digestive system, from fissures to reduced duodenal folds, despite the lack of symptoms. Studies have shown in severe cases it can take up to ten years for the digestive system to totally repair.
Not surprisingly, patients who had the most severe cases at diagnosis – in terms of histology and serology, not necessarily symptoms experienced – were the ones with the slowest recovery. However, even if you’re one of these patients where recovery happens on a slower pace, you are likely to feel a noticeable improvement in terms of symptoms and malabsorption parameters from the moment you embark on a gluten-free approach to food and control gluten exposure.
2. What if I don’t get better?
Most patients will experience a full recovery, even if it takes a few years. The control over gluten exposure is the key recovering your digestive tract. However, if you have been on a gluten-free diet for a while (6 to 12 months), but are still not showing signs of improvement, it may be time for you and your physician to go back to the drawing board and look closely at what may be inhibiting your recovery.
First, your doctor needs to re-assess your diagnosis of celiac disease. If the diagnosis is proved correct, then the next visit should be to your dietician to ensure that you’re not consuming products with gluten by accident. Unknowingly eating products with gluten is the most common cause for persistent symptoms and delayed recovery. You may be unknowingly ingesting gluten from cross contamination in the kitchen or work place eating area. Lastly, if all else fails, your physician may look for other reasons to explain your symptoms, such as pancreatic insufficiency, bacterial overgrowth or lymphoma.
If all these turn out to be negative, this is typically classed as refractory celiac disease. Treatment and follow-up in these cases can be challenging, as the condition is associated with a high risk of developing lymphoma in the long-term. Regular gastrointestinal endoscopies, as well as CT and PET scans are essential to screen these patients to detect any forms of cancer early.
3. How does my physician follow my progress?
As celiac disease is a chronic condition, your trips to the doctor don’t end at diagnosis. Patients with this condition face a lifetime of follow-up tests, to monitor progress and try to anticipate potential serious problems, such as increased risk of fractures or cancer. Or triggering other related autoimmune diseases.
The most important test to ensure intestinal healing is a follow-up biopsy, typically done at either 12, 24 or 36 months after diagnosis. Other exams include checking the levels of vitamin D, B6 and B12, folate, iron, calcium and phosphorus, to ensure no nutritional deficiencies develop; and tissue transglutaminase antibody (TTG) and deamidated gliadin peptide (dGp-IgG and dGp-IgA), used as markers of mucosal healing. Bone density scans should also be carried out at diagnosis and followed up yearly until an improving trend is obvious. The sixteen tests listed below is an example of the typical tests taken when following best practices. Knowing what tests to discuss with your doctor can be helpful in planning your follow up care. You doctor may not recommend all tests on the list or may suggest others tailored for your specific needs.
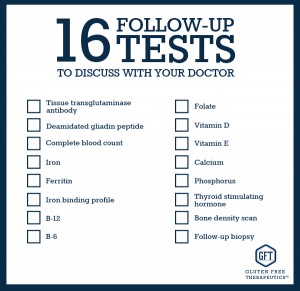 What’s important to note is that, more and more, instead of a one-fits-all approach, doctors are offering a personalised way to follow-up celiac disease patients based on their risk of complications. This way, patients at higher risk are seen more frequently than patients at low risk. This is beneficial not only for the patient, but also helps healthcare workers improve their patient care system. As with most chronic conditions celiac disease varies greatly among patients. It is good to know that the health care providers are recognising this and recommending treatment accordingly.
What’s important to note is that, more and more, instead of a one-fits-all approach, doctors are offering a personalised way to follow-up celiac disease patients based on their risk of complications. This way, patients at higher risk are seen more frequently than patients at low risk. This is beneficial not only for the patient, but also helps healthcare workers improve their patient care system. As with most chronic conditions celiac disease varies greatly among patients. It is good to know that the health care providers are recognising this and recommending treatment accordingly.
This original article is made possible by Gluten Free Therapeutics. Our mission is to educate, inform, and provide the most effective nutritional products possible to allow those with celiac disease and serious gluten intolerances to heal their bodies. CeliVites complete line of superior gluten free supplements includes multivitamin/multimineral supplements, iron supplements, and calcium supplements for people living with celiac disease. All CeliVites products are designed to help you heal, restore and rebuild your body, because going gluten free isn’t enough!
REFERENCES
- Biagi F, Gobbi P, Marchese A, Borsotti E, Zingone F, et al. Low incidence but poor prognosis of complicated coeliac disease: a retrospective multicentre study. Dig Liver Dis 2013, 46: 227-230
- Ciclitira PJ, King AL, Fraser JS. AGA technical review on celiac sprue. American Gastroenterological Association. Gastroenterology. 2001;120:1526–1540
- Grefte JM, Bouman JG, Grond J, et al. Slow and incomplete histological and functional recovery in adult gluten sensitive enteropathy. J Clin Pathol. 1988;41:886-891.
- Kaukinen K, Peraaho M, Lindfors K, et al. Persistent small bowel mucosal villous atrophy without symptoms in coeliac disease. Aliment Pharmacol Ther. 2007;25(10):1237–45.
- Krauss N, Schuppan D. Monitoring nonresponsive patients who have celiac disease. Gastrointest Endosc Clin N Am. 2006 Apr;16(2):317-27.
- Lebwohl B, Granath F, Ekbom A, et al. Mucosal healing and mortality in coeliac disease. Aliment Pharmacol Ther. 2013;37(3):332–9.
- Nijeboer P, van Wanrooij RL, Tack GJ, Mulder CJ, Bouma G. Update on the diagnosis and management of refractory coeliac disease. Gastroenterol Res Pract. 2013;2013:518483.
- Pekki H, Kurppa K, Mäki M et al. Predictors and Significance of Incomplete Mucosal Recovery in Celiac Disease After 1 Year on a Gluten-Free Diet Am J Gastroenterol. 2015 Jun 2. doi: 10.1038/ajg.2015.155. [Epub ahead of print]
- Rubio-Tapia A, Hill ID, Kelly CP et al. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 2013,108: 656–676
- Selby WS, Painter D, Collins A, et al. Persistent mucosal abnormalities in coeliac disease are not related to the ingestion of trace amounts of gluten. Scand J Gastroenterol. 1999;34:909-914.
- Uil JJ, van Elburg RM, van Overbeek FM, et al. Follow-up of treated coeliac patients: sugar absorption test and intestinal biopsies compared. Eur J Gastroenterol Hepatol. 1996;8:219- 223.
- Usta M, Urganci N. Does gluten-free diet protect children with celiac disease from low bone density? Iran J Pediatr. 2014 Aug;24(4):429-34.
- Vécsei E, Steinwendner S, Kogler H et al. Follow-up of pediatric celiac disease: value of antibodies in predicting mucosal healing, a prospective cohort study. BMC Gastroenterol. 2014 Feb 13;14:28.
- Wahab PJ, Meijer JW, Mulder CJ. Histologic follow-up of people with celiac disease on a gluten-free diet: slow and incomplete recovery. Am J Clin Pathol. 2002;118(3):459–463
Comments ()













Hi I am desperately looking for a dr in san Antonio? Been to 3 dr’s and told to eat wheat and it was in my head, I have and ferl worse but have no dr to guide me.
Thank you
Samantha
Hey, do yourself a favor and find a doc who specializes in Celiac, even if you have to travel out of state. I went to Columbia University in NY so I could get treated correctly. I live in NC and couldn’t find a specialist at Duke, Wake Forrest or UNC.
Cathy it’s a long way to California from Texas..lol i wish i could though.
it took two years but I am feeling normal again most of the time however, now I seem to be developing allergies to foods like Cherries and sometimes apples are irritating to my mouth. I also have chapped lips constantly, is this a side affect of Celiacs?
I have been diagnosed for 8 years and now if I bit into something with Gluten I feel a tight feeling in my throat, but have noticed that my sense of taste and smell are way off.